Think of a health issue that affects millions and a small fraction of women, is usually not diagnosed until years later, and may turn even a daily routine into a real challenge. It is what we call Polycystic Ovary Syndrome, or PCOS, in short. It is a silent struggle because its symptoms are confusing, humiliating and sometimes even despite them being apparent to everyone; it makes women feel lonely and misunderstood.
What is PCOS(Polycystic Ovary Syndrome)?
One may come across the term Polycystic Ovary Syndrome, and what may come into their mind immediately is the term cysts. It almost sounds like it is all about a growth on your ovaries, something that even hurts. And here is the shocking fact: PCOS is so much more than your ovaries or just cysts.
These are vital messengers referred to as hormones produced in your body continuously. They instruct various organs of your body on what to do, including how your heart should speed up, when you should feel hungry and they even tell you when your period is supposed to come. In PCOS, these two hormone tend to go crossed signals, and they are very essential ones
- Androgens (commonly known as male hormones) and women have them too, but with PCOS, you may wind up having too many. This may result in undesirable hair growth, pimples and even baldness all over.
- Insulin: This is a hormone that aids your body to use sugar as an energy source. Most women with PCOS have insulin resistance, that makes their bodies inefficient when using insulin. This leaves the body to produce even more insulin, which leads to yet more androgen production, which is rather confusing.
Due to such hormonal problems, your eggs may not come out at regular periods, translating into irregular periods. The so called cysts that people discuss are mostly just the young, ungrown egg sacs, which grew improperly.
Hidden Signs of PCOS
Here is why PCOS may be so hidden down battle:
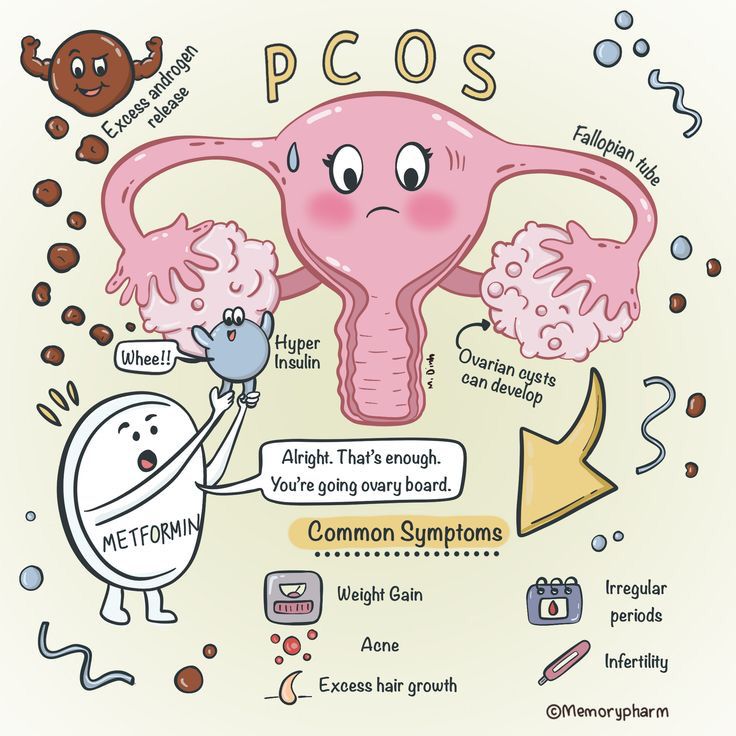
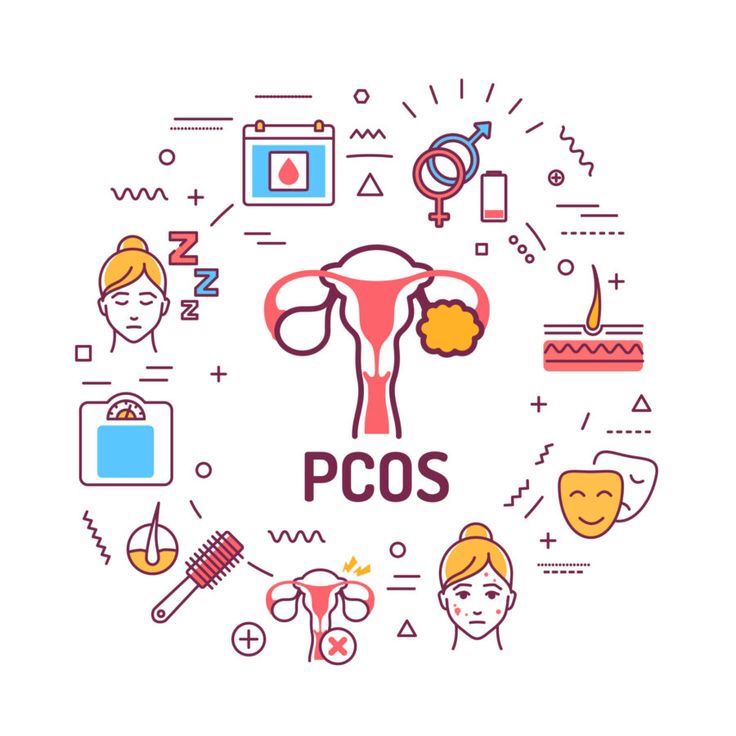
1. Irregular Periods
One of the most common ones is this. Your period can appear late, infrequently, or it simply does not come by. This is annoying, particularly when you want to get pregnant yet again simply in everyday life.
2. Hirsutism
In some cases, having unwanted thicker and darker hair on your face (chin, upper lip), chest or stomach may be very disturbing and even humiliating and a woman may spend a lot of money and time to cope with it without telling anyone.
3. Acne
Chronic acne (particularly on the jawline, the chin and the back) can surely take a toll on your self esteem.10 It is not only acne that teenagers have, but it may extend deep into adulthood.
4. Weight problems
Most women living with PCOS struggle a lot to lose weight particularly around their waists, even when they consume healthy food and perform exercises. This is usually associated with insulin resistance.
5. Hair Thinning
As your hair starts to grow, where you do not need it, the top of your head may start fading away especially society.
6. Fatigue and emotional status
The hormonal imbalance may result in woman always feeling tired and many women will feel anxious, depressed or have mood swings. This may be difficult to express to other individuals.
7. Infertile
This is because they may not ovulate (release and egg) regularly, and it may be harder to become pregnant. This can be devastating to women desperate to have a family.
8. The Hidden Battles
On top of the scarring, there is the rage, the perceived failure to be normal, the fear of condemnation, and there is there ceaseless seeking of solutions. A lot of women live in silence because they do not want to discuss these intimate matters.
According to International Research, Global Context
More than half of the cases of PCOS globally are not diagnosed even though the World Health Organization (WHO) believes that 8-13 percent of the world female population (of reproductive age) has the problem. Other international research show that the prevalence rate ranges between 5-21 percent. This implies that more than seven million women worldwide have PCOS and most of them are unaware of it.
Global Contributors to PCOS
Unhealthy lifestyles have been identified as one of the key causes of PCOS globally. International guidelines, including those sponsored by well-known organizations, such as the European Society of Human Reproduction and Embryology (ESHRE) and the American Society for Reproductive Medicine (ASRM) , insist strongly on lifestyle changes as the initial method of managing PCOS, which focuses on a proper diet and physical activity.
The emotional impact of PCOS is also a real thing, no matter where you live in the world. . Mental complications and PCOS are one of the factors that concern healthcare providers across the globe.
Fertility Problems around the World
PCOS is known to present the highest rates of an ovulatory infertility (the inability to release an egg) in the world. The greatest figure on the rate of infertility, as an April 2023 research by WHO showed, remains at about 17.5 percent in the world (1 in 6 adult population is infertile). PCOS presents a huge burden to the global infertility crisis.
International Organization (e.g. UNICEF)
Although UNICEF mostly relates to children rights and welfare, they also contribute indirectly to women health. One example is around menstrual health and hygiene (MHH) issues where UNICEF may partner with local non-governmental organizations (NGOs) (such as Santex in Pakistan) to improve MHH and to create awareness of issues related to menstruation Even here, identification of young girls with irregular periods which may be an indication of PCOS may be an indirect result due to increased awareness about menstrual issues.
Pakistan research Context
PCOS is very common in Pakistan as studies have been done in various areas of the country, most of them indicating that PCOS prevalence in Pakistani women could reach as much as 52% of the overall population; when using wider diagnostic criteria or in certain groups. Others indicate that the incidence of PCOS is around 19-31 percent in young women and student. Such figures are frequently even greater than those of Western nations, which make the local concern and eyewear policies important.
Urban vs Rural Trends (Pakistan)
A study done by Pakistan researchers indicated that PCOS prevalence may be higher in acceptably in urban population. A study conducted among adolescent girls revealed that urban adolescents were more likely to have PCOS (34.1 percent) than rural adolescent girls (19.0 percent). This might be correlated with some lifestyle factors, such as eating habits and exercise activity frequently connected with the process of urbanization.
The Effect of Lifestyle in Pakistan
Local research proves and conclusions have been reached stating that the association between PCOS and their lifestyle is great. In Pakistani studies, they have discovered that activities such as lack of exercise in females, the use of fast food regularly, and sleep deprivation were highly associated with PCOS in girls aged 13 to 16 years. Irregular meal pattern and extensive consumption of junk food are reported among other female PCOS patients as well. This can be taken to stress that even small things such as a change in daily regimes can change things and help women with PCOS in Pakistan.
Psychological consequences of PCOS in Pakistani Women
The psychological effects of PCOS are very profound as an overwhelming majority of PCOS affect women in Pakistan are lonely (55%), anxious (65%), and depressed (45%) though the results demonstrate a high incidence of every single psychological symptom in all the cities where the survey was conducted. Women may be sought to be discouraged further by a social stigma on speaking out about their health.
Hormonal Profile in Pakistani Women
Local researches always validated the general knowledge regarding the hormonal imbalances with regard to PCOS. In Pakistan, women with PCOS have been shown to have high levels of androgens (such as testosterone), increased LH/FSH ratios and a large degree of insulin resistance. This means that the hormonal fundamentals of PCOS are similar here, but the degree to which they affect you can be affected by local genetic and environmental factors.
Fertility Issues in Pakistan
PCOS is one of the leading causes of problems getting pregnant to many women in Pakistan. Female infertility is also a profound problem in Pakistan, and 21.9 percent of all couples are affected. Moreover, PCOS is one reason of female infertility that is widely spread, as it causes such an issue in 38.5 percent of cases. This implies that a good number of PCOS women in Pakistan have the extra emotional burden of childlessness unless they resort to fertility treatments. Experts remark that PCOS has become a silent epidemic that causes infertility and miscarriages in Pakistani women and the elevated rates are typically associated with the such issues as obesity and sedentary life styles.
Diagnosis of PCOS
The health history, a physical exam along with a certain test are used when diagnosing PCOS (Polycystic Ovary Syndrome). One must keep in mind that PCOS can be a diagnosis of exclusion which means that other diseases with similar symptoms have to be dismissed prior to making this diagnosis.
1. Clinical Assessment
- Symptoms: Your physician may inquire regarding the development of irregular periods or no periods, and the presence of high male hormones such as extra body/facial hair, pimples, or hair loss.
- Physical Exam: Under this section, they will examine whether you are affected by the following physical signs and check your blood pressure and weight.
2. Blood Tests
The tests play a significant role in determining the level of the hormone and performing any related metabolic disease. In theory, these are supposed to be at the early follicular part of your monthly (it is around the 3 days) in case you have periods and are not using the hormonal birth control (you might want to pause it 3 months before).
Hormone Panel
- Total and Free Testosterone: In PCOS, it is a critical feature to the increase in testosterone level as a sign of hyperandrogenism. The form that is biologically active is free testosterone.
- Sex Hormone-Binding Globulin (SHBG): Low levels of SHBG may also cause an increase in free testosterone despite normal states of total testosterone.
- Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH): an abnormally high ratio of LH to FSH occurs in some women with PCOS, although it is not so reliable as it used to be.
- Prolactin: It needs to be excluded that the elevated levels of prolactin are the cause of irregular periods.
- Thyroid-Stimulating Hormone (TSH) and Free Thyroxine (T4): It should be done to exclude thyroid dysfunction because it can produce the similar symptoms of PCOS (e.g., irregular menstrual periods, weight changes).
- Dehydroepiandrosterone Sulfate (DHEA-S) and Androstenedione: These are other androgens which can be raised during PCOS.
- Anti-Mullerian Hormone (AMH): AMH has been detected to be high in PCOS and associated with the abundance of small ovarian follicles. It may serve as a convenient diagnostic indicator, acting even as a replacement of an ultrasound in specific instances.
Metabolic Screening
- Fasting Glucose and Insulin: To check presence of insulin resistance that is typical of PCOS.
- HbA1c: To take a typical number of how much sugar exists in your blood in the last few months, screening of pre-diabetes or type 2 diabetes.
- Lipid Profile: Cholesterol (total, LDL, HDL) and triglycerides are all tested to determine whether women with PCOS are at higher risk of a cardiovascular disease.
3. The use of Imaging (Pelvic Ultrasound)
It scans to look at the presence of uneven/polycystic ovarian morphology (PCOM) which is the presence of many small and poorly developed follicles in the ovaries, and evaluates the size of ovaries. It also rules out the lining of the uterus.
Note: You may not always require an ultrasound when other indications are evident particularly on the youth.
Diagnosis Criteria
They are normally diagnosed when you have at least two out of the following three (called Rotterdam Criteria) once all other conditions have been eliminated:
- Abnormal or missed periods (which means not very frequent or non occurring ovulation).
- Indication of too much male hormone (hirsutism/acne or high levels of androgen on blood tests).
- The presence of 12 or more follicles each with a diameter of 29 mm in at least one ovary and/or an ovarian volume more than 10 mL defines this. It should be remembered that the exact number of follicles for diagnosis has been debatable and revised; recent guidelines recommend a threshold of ≥20 follicles per ovary, or perhaps ≥25 follicles. Because of the high prevalence of multifollicular ovaries in this age group, ultrasound should usually not be used for diagnosis in adolescents (within eight years of menarche or under 20 years old).
Management of PCOS
1. First Line: Lifestyle Changes
- Diet: restricting processed foods and refined sugars, balanced, nutritious, high fiber.
- Exercise Regular aerobic and strength training can help manage weight and raise insulin sensitivity.
- Weight Control: Vital for symptom reduction; even small weight loss helps.
- Stress Management: Methods include yoga, meditation, and enough sleep.
2. Medicines (Consult your Doctor)
- For Menstrual Irregularity & Hyperandrogenism (Hirsutism, Acne, Hair Loss).
- Hormonal treatments aim to control periods and lower androgen effects.
- Specific medications to block androgen effects for severe symptoms.
- Regional treatments for facial hair.
- Medication to increase insulin sensitivity might help to control weight and menstruation.
- Oral drugs to promote ovulation.
- Injectable hormone treatments should be used if oral options are ineffective.
- Surgical operations (in certain circumstances).
3. Long Term Health Control
- For Type 2 Diabetes, high blood pressure, and high cholesterol. Regular screening is required.
- Methods for ensuring normal shedding of the uterine lining are known as endometrial protection.
- Treat body image issues as well as anxiety and depression.
- Particularly for those who are overweight or obese, sleep apnea screening.
Key Notes:
- Though treatable, PCOS is chronic and has no cure.
- Management is very personal and usually calls on a group of healthcare professionals.
- Patient education and continuing assistance are essential.
- Always seek personalized advice from a medical expert.

 Medically reviewed by
Medically reviewed by