Did you realize that 38.4 million Americans are affected by type 2 diabetes? This condition may have huge impacts on your life unless dealt with. A good approach to having diabetes mellitus type 2 is to change your lifestyle, monitor your health, and, occasionally, use some medication. In this guide, we will consider the effective methods to regulate your blood sugar level and improve your health. The knowledge of your condition and how it can be beneficial to effectively manage it will give you the authority to control your own health and make wise decisions regarding your health.
Understanding Diabetes Mellitus Type 2
To help you cope with type 2 diabetes, it is important to be aware of the changes it produces. It is a metabolic condition that disrupts your body’s metabolism of glucose, the main energy source.
What Happens in Your Body with Type 2 Diabetes?
In type 2 diabetes, your body does not react to insulin as it does. Insulin is one of the regulating hormones of blood sugar levels. Thus, the glucose remains in your blood rather than entering cells to create energy.
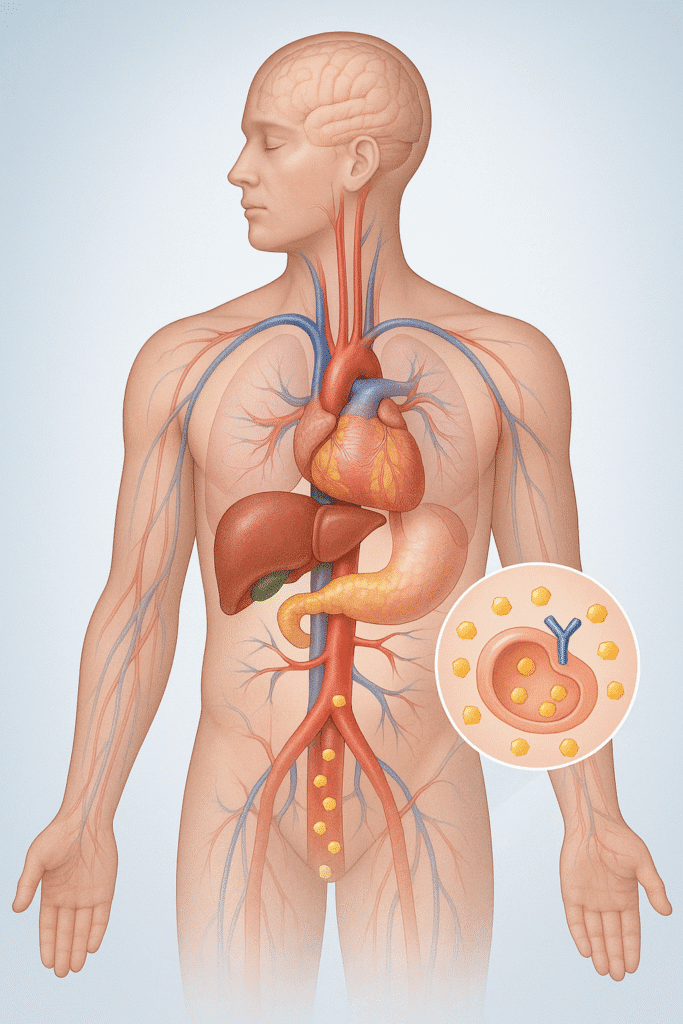
This will have the effect of increasing blood sugar over time. It has a lot of possibilities to damage numerous organs and systems in your body.
Difference between Type 1 & 2 Diabetes
Type 1 diabetes occurs when your body destroys insulin producing cells that are located in your pancreas. This implies that you do not produce much insulin. Type 2 diabetes, on the other hand, is all about your body not using insulin productively. It is usually associated with lifestyle and genetics.
| Feature | Type 1 | Type 2 |
| Onset | Sudden | Gradual |
| Age | Usually young | Usually 40+ (but increasing in youth) |
| Body weight | Often normal | Often overweight/obese |
| Insulin production | None | Decreased/resistant |
| Treatment | Always needs insulin | Diet, exercise, medications, sometimes insulin |
| Cause | Autoimmune | Lifestyle factors and genetics |
Causes and Risk Factors
Several factors affect you:
1. Weight: A recent study discovered that you are at the greatest risk of being overweight as well as weighing more than your middle. Insulin becomes resistant in your body due to fat cells.
2. Lack of activity: When you lack activity but go around expecting things to happen with you, you are inviting trouble. Physical activity prevents obesity and burns glucose in the form of energy.
3. Genes: Do you have family with diabetes? The chances of your risk increase. Your chances rise even more when you have it in both parents.
4. Age: The older you are, the more at risk you are, particularly after 45. Your pancreas is exhausted, and your muscles are more ineffective.
5. Race/ethnicity: There is a level of increased risk, in other groups Black, Native American, Hispanic, people, as well as Asian-American people develop Type 2 diabetes more often.
6. Dietary intake: Are you consuming too much sugar, unprocessed food, and lacking adequate fiber? That is a formula for insulin resistance.
7. Stress and sleep: Sleep deprivation and constant stress affect your hormones and blood sugar levels.
Symptoms of Type 2 Diabetes
These are red flags to watch out for:
- Incessant thirst and even having as much water as you can, you always feel thirsty
- Taking frequent bathroom trips, particularly at night
- Weight loss (despite the intake of a regular diet)
- Constant hunger on and after eating
- Fatigue that does not improve even after resting
- Intermittent Blurred vision
- Scars and bruises that last forever to heal
- Head-to-toe tingling or numbness of hands and feet
- Frequent skin infections or itching of the skin
Complications When Untreated
The problem of high blood sugar is that it will harm the blood vessels and the nerves all over the body:
1. Heart Disease and Stroke
With diabetes, you are two times more exposed to this risk than individuals who do not have it. Heart attacks tend to strike earlier and more often.
2. Kidney Damage
A high blood sugar level may cause damage to the kidneys, with their millions of minute vessels in which the blood is filtered. This may cause kidney deficiency and require dialysis.
3. Neuropathy (Nerve Damage)
So, it is not tingling and numbness, and burning pain as minor nuisances. They are indications that your nerves are being destroyed. That may cause the injuries that you cannot feel, and ultimately, amputations.
4. Eye Damage
The number one cause of new vision loss in adults occurs in diabetes. Your small blood vessels in your retina are destroyed, and this causes diabetic retinopathy.
5. Foot Problems
It leads to poor ability to heal infections in response to poor circulation and nerve damage, which makes your feet susceptible to infections. Minor issues may turn out to be severe.
6. Skin Diseases
Bacteria and fungi thrive in sugary conditions produced by diabetes.
7. Impairment
Diabetes can cause hearing difficulties.
8. Alzheimer’s
The correlation between dementia and Type 2 diabetes has been shown.
ICD-10 Diabetes Type 2 and Complications
Where doctors report about Type 2 diabetes with complications, they apply certain codes of the ICD-10 classification system. They are useful in diagnosis, treatment planning, and insurance.
The Type 2 diabetes code foundation code is E11, yet complicated cases of diabetes are identified by several extra figures:
• E11.2: Kidney Complications (with nephropathy)
• E11.3: Complications of the eye (retinopathy)
• E11.4: Neurological Complications (neuropathy)
• E11.5: Circulatory complications
• E11.6: Other specified complications
• E11.8: Unspecified complications
• E11.9: Without complications
The importance of these codes is that they assist in keeping the progression of diabetes’s impact on the various body systems on track, and they also determine the correct ways to treat all the complications. When you see that your medical records contain these codes, it is an indication that your healthcare provider is keeping track of certain problems related to diabetes.
How to Manage the Effects of Diabetes Mellitus Type 2 Effectively?
By fully understanding type 2 diabetes as a chronic condition, you can find ways to manage its effects on your health, well-being, and way of life effectively.
Creating Your Personalized Diabetes Control Plan
To manage your blood sugar successfully, you must have a program. This is a plan that your healthcare team should be working on. They will ensure that it suits your needs and health objectives.
Working with your Health Professionals
Your medical team plays an important role in controlling your diabetes. These people might be your doctor, a dietitian, or an endocrinologist. You should regularly meet with them to keep track and make the necessary changes.
Setting Targets of Blood Sugar Control
One area that is significant in the management of diabetes is setting attainable goals. These goals have to be exact, measurable, and associated with your health objectives. An example would be that you would like to have a specific HbA1c or improved glucose monitoring. The big goals can be achieved with smaller steps, and hence are simple to manage.
| HbA1c Level | Less than 7% | 3 months |
| Fasting Blood Glucose | 70-130 mg/dl | 2 months |
| Physical Activity | 150 minutes/week | 1 month |
How to Monitor Your Progress and the Steps of Adjusting?
It is important to monitor your blood sugar, diet, and exercise. This can be eased by using a diabetes logbook or a mobile application. With your development, you, as well as your team, can make adaptations in your plan.
These steps can help you make a diabetes management plan that will help you live better and manage your blood sugar levels.
Nutritional Strategies for Blood Sugar Control
Control over type 2 diabetes requires smart eating. Proper diet also maintains stabilized blood sugar. It enhances your health and happiness as well.
1. What are Carbohydrates and GI?
Carbs influence your blood sugar a lot. The important thing is to know the Glycemic index (GI) of the foods. Low GI foods such as grains and vegetables take a long time to digest. This causes the gradual elevation of blood sugar.
By choosing low GI foods, it is possible to regulate the sugar in the blood. Keep in mind that the glycemic load also counts. It looks at the amount of carbs in a serving of food.
2. Meal Planning and Portion Control
It is essential to plan your meals in case of diabetes. A balanced diet maintains blood sugar at a moderate level. Another crucial aspect is portion control, as it regulates carbs and calories.
The following are some of the meal planning tips:
- Consume a diversified diet, with the inclusion of veggies, fruits, whole grains, lean meat, and healthy fats.
- Monitor the levels of carbs in your snacks and meals.
- Measure food in measuring cups or using a food scale.

3. Beneficial Foods that are Diabetes Friendly
Some foods are more useful in dealing with diabetes. These include:
- High-fiber Choices
- Legumes, oats, and barley are also foods rich in fiber. They retard carb digestion, which keeps the sugars in the blood at bay.
- Good Fats and Proteins
- Inclusion of healthy fats such as avocados and nuts, and low-fat products such as poultry and fish can sustain you. They equally contain essential nutrients.
4. Limited or Avoided Foods
Certain foods are dangerous to both blood sugar levels and health. One should limit or eliminate:
- Additional foods such as sugary beverages and food.
- Finished complex carbs, e.g., white bread and ready snacks.
- Saturated and Trans fat foods.
Weight Management Role in diabetes Control
Weight management is an important factor in maintaining type 2 diabetes. In case you have type 2 diabetes, your body is not good at using insulin. Such is associated with elevated sugar levels in the blood. Weight loss can enhance your body’s response to insulin and manage your diabetes.
1. The Connection between Insulin Resistance and Weight
Insulin resistance occurs when the body fails to react to insulin well in the cells. You may therefore become insulin resistant when you are overweight and or when your belly is overweight. In cases of being overweight, the fat cells produce some substances that can interfere with the insulin messages. This reduces the ease with which glucose can enter your cells, increasing your blood sugar levels.
2. How much Weight loss Can Impact Your Diabetes?
Losing even a few pounds will assist in regulating your diabetes. It is possible to have insulin sensitivity and lower your blood sugar by losing 5-10 per cent of your body weight. For example, when you weigh 200 pounds, the loss of 10-20 pounds may make a lot of difference.
- Weight loss improves insulin sensitivity: Essentially, it has been seen that weight loss achieves this goal by enhancing how the cells of the body respond to insulin.
- Reduced Blood Sugar Levels: With increased sensitivity of the body towards insulin, the blood sugar levels are reduced.
- Reduced Medication Weight loss can result in a decrease in the intake of medication in diabetes.
3. Sustainable Strategies of Weight Management
To lose and maintain weight, you must have a long-term plan. The following are some of the strategies:
1. Eating Right: Enjoy a diverse diet containing heaps of vegetables, fruits, whole grains, lean protein, and healthy fat.
2. Physical Activity: Get 150 minutes of moderate intensity aerobic activity or 75 minutes of vigorous intensity aerobic activity or a combination of both per week.
3. Follow-Up: Weigh, measure, and take your progress pictures to keep you motivated.
Exercise Recommendations and Physical Activity
Exercise plays an important role in the management of Type 2 diabetes. It increases insulin sensitivity and decreases the risk of complications. Exercise also regulates the sugar levels in the blood and ensures general fitness.
1. The Advantages of Routine Exercise on Glucose Management
Type 2 diabetes benefits from a lot of regular physical activity. It contributes to muscle in fluxing to glucose and to enhancing the consciousness of insulin and diminishing the body fat. The latter contributes to glucose control and a reduction in the risk of complications.
The main advantages are the following:
- Better Insulin sensitivity
- Improved glucose tolerance
- Weight management
- Decreased chance of cardiovascular disease
2. Types of Exercise for Diabetes Control
These include aerobic exercise, strength training, and flexibility/Balance activities as the major ones.
Working out using aerobic activities such as swimming, biking, or walking is excellent for the maintenance of the heart and glucose control. Intend to exercise 150 minutes of moderate-intensity aerobics a week.
Strength Training
Strength training causes one to gain muscle, increasing insulin sensitivity. Perform strength training once every two days by working out every large muscle group.
Activities involving Flexibility and Balance
Employment of activities such as yoga or tai chi enhances physical functionality, reduces the risk of falls, and increases flexibility.
| Exercise Type | Benefits | Examples |
| Aerobic Exercise | Improves cardiovascular health, enhances glucose management | Walking, cycling, swimming |
| Strength Training | Builds muscle mass, improves insulin sensitivity | Weightlifting, resistance band exercises |
| Flexibility and Balance | Improves flexibility, reduces fall risk | Yoga, tai chi |
Medication and Insulin Therapy Options
To most individuals affected with type 2 diabetes, their care is incomplete with medication and insulin. One should be aware of the available treatment.

Oral Medicines
Type 2 diabetes has oral medicines, which are normally the first line. They do this in different ways, such as increasing the release of insulin or enhancing the effectiveness of insulin in the body.
Typical Oral Drugs
• Metformin: Suppresses the production of glucose by the liver.
• Sulfonylureas: Cause the pancreas to secrete insulin at an increased rate.
• DPP-4 inhibitors: Assist in controlling blood sugar levels by controlling insulin and glucose.
Insulin Therapy Use, When and How
Insulin injection is applied when oral drugs fail to normalize the blood sugar. It happens through injections or an insulin pump. The insulin therapy can be modified, and various types include rapid-acting insulin and long-acting insulin.
Average Insulin Dosage of Type 2 Diabetes
The key concern in managing blood sugar is the presence of the right dosage of insulin. Does it depend on the weight, level of activities, and health conditions?
| Type of Insulin | Typical Dosage | Timing |
| Rapid-acting | 5-10 units | Before meals |
| Short-acting | 10-20 units | 30 minutes before meals |
| Long-acting | 20-40 units | Once or twice daily |
Managing your Condition Effectively
Knowledge of how to manage diabetes in type 2 is important in terms of the way you watch over your condition. Effective observation helps you to make intelligent decisions concerning your care. This will enable you to manage levels of glucose in your body and make you healthier.
Blood Glucose Monitoring Techniques
Diabetes monitoring is done through blood glucose monitoring. You find out your blood sugar at different times using a glucometer. Monitoring regularly demonstrates the way your body behaves towards food, exercise, and medicine. This allows you to make the appropriate changes.
- Monitor your blood glucose level as instructed by your health coach.
- Log your readings and follow patterns and trends.
- Correct your diet, exercise, or medication according to your glucose reading
Understanding about A1C and other main indicators
The A1C test depicts the 2-3 month blood glucose levels. It is a useful instrument to determine whether your diabetes plan works. Such significant indicators are fasting glucose and postprandial glucose.
What Makes a Good Glucose Management Indicator?
A good glucose management indicator provides useful and valid information. It is expected to assist you in viewing your glucose patterns and making care decisions. A1C test and frequent blood glucose monitoring present the complete picture of your glucose care.
Technological Use in Improved Management of Diabetes
The use of technology is increasingly becoming significant in diabetes management. Such tools as the continuous glucose monitors and diabetic applications assist in measuring and managing your condition.
1) Non-Stop Glucose Monitors
Continuous glucose monitors (CGMs) monitor your level of glucose throughout the day and night. They provide real-time information and warnings on high or low glucose.
2) Diabetes Management Apps
Diabetes tracking applications allow you to record your glucose levels and monitor your food intake and physical exercise. They also check up on your medication. There are a great number of apps containing insights and suggestions as to how you can better manage your diabetes.
Conclusion
To control type 2 diabetes effectively, one has to make major lifestyle changes. It implies collaboration with your doctor and monitoring your health. In this way, you will be able to manage your blood sugar. When you have type 2 diabetes, you should be smarter with what and how you eat and move. Adhering to a healthy habit may reduce the chances of major complications. It also lets you live a better life in general. It is important to learn nutrition, weight management, and exercise. These are the habits that assist you in managing your diabetes. You can incorporate them into your daily life, where you live healthier and happier.

 Medically reviewed by
Medically reviewed by