Ever had a “gut feeling” about something? Turns out, your gut really might know best. For years, scientists have been uncovering the fascinating link between your digestive system like gut and mental health and it’s deeper than we ever imagined. Your gut isn’t just for digesting food; it’s actually your “second brain,” loaded with neurons and bacteria that can influence how you feel, think, and act.
What is the Gut-Brain Axis?
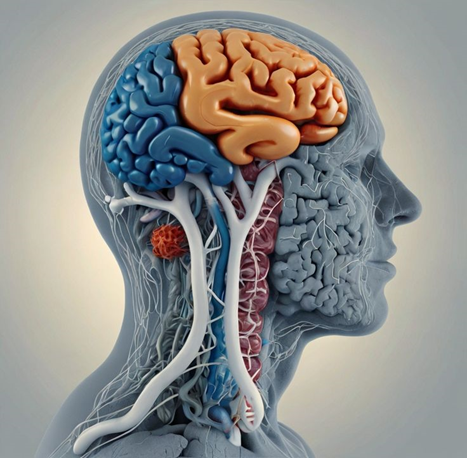
The gut-brain axis is the two way communication system between your central nervous system (your brain and spinal cord) and your enteric nervous system (the massive network of neurons lining your gut). It’s like a hotline that keeps your brain and digestive system in sync.
How the Brain and Gut Communicate?
The brain and gut are closely connected through a bidirectional communication system known as the gut-brain axis. This system relies on three main pathways: electrical signals, chemical messengers, and hormones. Together, these components allow the central nervous system (CNS) and the enteric nervous system (ENS) in the gut to exchange information continuously.
- Electrical Signals
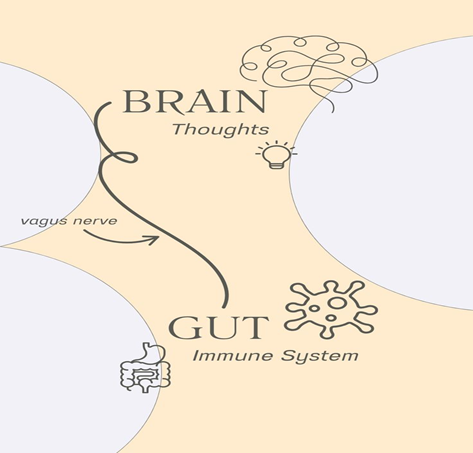
The vagus nerve is a key player in transmitting electrical impulses between the brain and the gut. It is the longest cranial nerve and acts like a communication highway, carrying information about gut activity such as inflammation, nutrient content, and microbial presence directly to the brain. - Chemical Messengers
The gut contains millions of neurons and produces neurotransmitters, such as serotonin, dopamine, and gamma-aminobutyric acid (GABA). In fact, around 90% of the body’s serotonin is made in the gut. These chemicals play essential roles in regulating mood, anxiety levels, and emotional responses. Changes in gut activity or microbiota can alter neurotransmitter levels, directly influencing how the brain functions. - Hormones
The gut also secretes hormones like cortisol, ghrelin, and leptin, which affect stress response, appetite, and energy regulation. These hormones enter the bloodstream and can signal the brain to adjust physiological and behavioral responses accordingly.
Role of the Vagus Nerve
The vagus nerve plays a central and essential role in the gut-brain axis, acting as the primary communication pathway between the gut and the brain. Originating in the brainstem, it extends down into the chest and abdomen, directly connecting with major organs, including the stomach and intestines.
This nerve carries a mix of sensory and motor fibers, enabling it to both send signals from the gut to the brain (afferent signals) and transmit instructions from the brain back to the gut (efferent signals). Roughly 80–90% of the vagus nerve’s fibers are sensory, meaning most of the information flows from the gut upward to the brain.
When the gut is experiencing inflammation, infection, or microbial imbalance, the vagus nerve detects these changes through specialized receptors in the gut lining. It then rapidly communicates this information to the brain, particularly to regions involved in mood regulation, pain perception, and the stress response, such as the hypothalamus and limbic system.
Meet the Microbiome
What is the Gut Microbiome?
The gut microbiome refers to the vast community of microorganisms primarily bacteria, but also including viruses, fungi, and archaea that live in the digestive tract, especially the large intestine. These microbes coexist with the human body in a symbiotic relationship, meaning they benefit from living in the gut while also performing essential functions that support our health.
Each person’s gut microbiome is unique and contains trillions of microbes, collectively weighing up to 2–3 pounds. Although invisible to the naked eye, these organisms play a powerful role in:
- Digesting complex food components, such as fiber, which the body cannot break down on its own.
- Producing vital nutrients, including certain B vitamins and vitamin K.
- Training and regulating the immune system, helping the body distinguish between harmful invaders and harmless substances.
- Maintaining the gut barrier, preventing toxins and pathogens from entering the bloodstream.
- Influencing brain function and mood through the production of neurotransmitters and interaction with the gut-brain axis.
How Gut Bacteria Influence Brain Function?
Some bacteria in your gut can make important brain chemicals called neurotransmitters, like serotonin, dopamine, and GABA. These chemicals help control your mood, sleep, and stress levels. In fact, around 90% of your body’s serotonin which helps you feel calm and happy is actually made in the gut, not the brain. Certain good bacteria, such as Lactobacillus and Bifidobacterium, help produce these mood-regulating chemicals.
These gut made chemicals affect the brain through different pathways, like the vagus nerve and immune system signals. Even if they don’t always travel directly to the brain, they still send messages that can change how you feel and think. This is why having a healthy balance of gut bacteria is so important not just for digestion, but also for your mental health and emotions.
Microbiome Diversity and Mental Wellness
A healthy gut is a diverse gut. A wide variety of beneficial bacteria helps reduce inflammation, boost immunity, and support a balanced mood. When diversity shrinks, mental health tends to take a hit.
The Science Linking Gut Health to Mental Health
Human Studies
1. Systematic review (May 2025)
A comprehensive review analyzed 24 clinical studies and found that pro inflammatory bacteria (e.g. Proteobacteria, Enterobacteriaceae, Fusobacterium) are increased, while anti-inflammatory, short chain fatty-acid (SCFA) producing bacteria (e.g. Faecalibacterium, Lachnospira, Butyricicoccus) are reduced in individuals with depression or anxiety.
2. Anxiety-specific microbiome review (2024–2025)
Smaller studies in individuals with generalized anxiety disorder (GAD) show a consistent depletion of beneficial taxa like Eubacterium, Coprococcus, and Faecalibacterium, along with lower microbial diversity.
Animal & Transplant Studies
3. Fecal microbiota transplants from depressed humans
Transferring stool from depressed patients into germ free rats resulted in noticeable depressive behaviors, supporting a causal link.
4. Social anxiety disorder (SAD) bacterial transfer
Mice receiving gut microbiota from SAD patients displayed increased social fear, providing direct behavioral evidence of gut-driven anxiety.
5. SCFA vagus signaling models
Theoretical modeling shows that SCFAs metabolites from gut bacteria can activate vagal nerve pathways affecting brain signals, offering mechanistic insight into gut-brain communication.
Inflammation and Mood Disorders
An imbalanced gut can lead to systemic inflammation, which has been linked to depression, anxiety, and even bipolar disorder. Chronic inflammation messes with brain chemistry and function over time.
Gut Health and Anxiety
How Dysbiosis Contributes to Anxiety?
Dysbiosis happens when harmful bacteria in your gut outnumber the good ones. This imbalance can cause inflammation in the body and damage the gut lining, allowing unwanted substances to enter the bloodstream. These substances can affect the brain and increase feelings of stress and anxiety. The gut and brain are closely linked, so when your gut is unhealthy, it can directly impact how you feel emotionally.
Dysbiosis can also reduce your body’s ability to absorb important nutrients like vitamin B12, magnesium, and tryptophan nutrients needed to make neurotransmitters like serotonin and GABA, which help keep you calm and balanced. When the gut can’t produce or support these brain chemicals properly, it can lead to mood problems, including anxiety.
Gut Based Strategies for Managing Anxiety
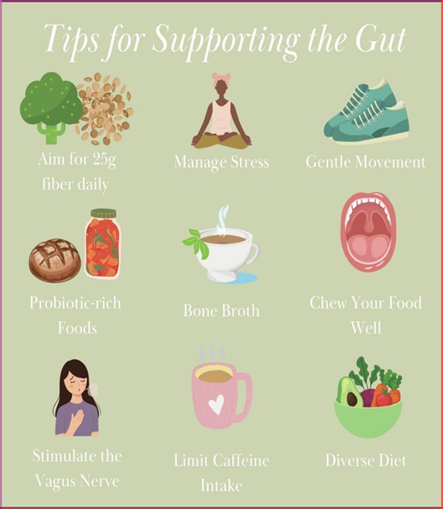
Eat a Gut Friendly Diet
- Include fiber rich foods like vegetables, fruits, legumes, and whole grains.
- Add fermented foods (e.g., yogurt, kefir, kimchi, sauerkraut) to support beneficial bacteria.
- Avoid processed foods, added sugars, and artificial sweeteners, which can harm gut balance.
Take Probiotics
- Use probiotic supplements with strains like Lactobacillus and Bifidobacterium.
- These can help improve mood by supporting neurotransmitter production and reducing inflammation.
Practice Stress Reduction Techniques
- Meditation and mindfulness calm the mind and reduce gut-related stress.
- Deep breathing activates the vagus nerve, which helps regulate the gut-brain connection.
Support the Vagus Nerve
- Stimulate it naturally through cold exposure, humming, or slow diaphragmatic breathing.
- A healthy vagus nerve improves communication between your gut and brain, helping reduce anxiety.
Gut Health and Depression
Link Between Gut Imbalance and Depression
People with depression often have higher levels of harmful bacteria and lower levels of beneficial ones. These shifts can lead to poor neurotransmitter production and increased inflammation.
Success Stories from Research Trials
1. 2022 Multi Strain Probiotic in Major Depression
A randomized, double‑blind, placebo‑controlled trial published in Translational Psychiatry in 2022 investigated the effects of an 8-week, daily multi strain probiotic supplement in individuals with moderate depression. The probiotic group showed significant reductions in depression scores, comparable to typical pharmacological outcomes. You can explore the full study for detailed methodology and results.
2. 2023 Lactobacillus & Bifidobacterium in Stressed Young Adults
A 2023 trial featured in Nutrients examined the impact of a combined Lactobacillus and Bifidobacterium probiotic on mood, anxiety, and sleep among young adults under stress. Participants experienced notable improvements in mood, reduced anxiety scores, and better sleep quality after the intervention.
Microbiome and Neurodegenerative Diseases
When there’s an imbalance in gut bacteria called gut dysbiosis it can cause inflammation and harmful substances that may reach the brain. This might play a role in brain diseases like Alzheimer’s, Parkinson’s, and multiple sclerosis.
For example, in Parkinson’s disease, harmful proteins have been found in the gut before they appear in the brain. These may travel along the vagus nerve, which connects the gut and brain. In Alzheimer’s, poor gut health might reduce helpful brain-protecting substances.
The Diet Mood Connection
Mood Boosting Foods for Gut and Brain
- Leafy greens
- Fatty fish
- Whole grains
- Nuts and seeds
- Berries
These are packed with nutrients and fiber that support both gut and brain function.
Fermented Foods and Prebiotics
Yogurt, kefir, sauerkraut, kimchi, and miso are your gut’s best friends. Prebiotics like onions, garlic, and bananas feed the good bacteria and help them thrive.
Lifestyle Factors That Affect the Gut-Brain Axis
Several everyday habits can strongly influence how well your gut and brain work together. These include:
- Diet
Eating a diet high in processed foods, sugar, and unhealthy fats can harm gut bacteria. A fiber-rich, plant-based diet supports a healthy microbiome and improves brain function. - Sleep
Poor sleep disrupts gut bacteria and weakens the gut-brain connection. Getting 7–9 hours of quality sleep each night helps both your gut and mental health. - Stress
Chronic stress can damage the gut lining, cause inflammation, and reduce healthy gut bacteria. Managing stress through mindfulness, deep breathing, or physical activity can help restore balance. - Physical Activity
Regular exercise supports healthy digestion, boosts beneficial gut bacteria, and improves mood by increasing brain-friendly chemicals like endorphins. - Antibiotic Use
Frequent or unnecessary antibiotic use can wipe out both good and bad bacteria, disrupting gut balance. Always use antibiotics only when prescribed. - Hydration
Drinking enough water supports digestion and helps maintain a healthy gut environment.
Probiotics, Prebiotics, and Psychobiotics
Here is a clear table explaining Probiotics, Prebiotics, and Psychobiotics, along with their definitions and differences:
| Term | Definition | Main Function | Sources/Examples |
|---|---|---|---|
| Probiotics | Live beneficial bacteria that support a healthy gut microbiome. | Restore or maintain good gut bacteria. | Yogurt, kefir, kimchi, probiotic supplements |
| Prebiotics | Non-digestible fibers that feed beneficial gut bacteria. | Help probiotics grow and stay active. | Garlic, onions, bananas, oats, asparagus |
| Psychobiotics | Specific probiotics or prebiotics that have a mental health benefit. | Improve mood, reduce anxiety and stress through the gut-brain axis. | Lactobacillus and Bifidobacterium strains; fiber-rich foods like inulin |
What to Look for in a Supplement?
When choosing a probiotic supplement, it’s important to focus on quality, potency, and effectiveness. Look for products that contain multiple strains of beneficial bacteria, such as Lactobacillus and Bifidobacterium. A combination of strains can support different aspects of gut health and may have broader benefits for digestion, immunity, and mood.
The supplement should also provide at least 10 billion CFUs (colony-forming units) per serving. This ensures there are enough live bacteria to survive stomach acid and reach the intestines where they’re needed. Finally, check that the product guarantees viability through the expiration date, not just at the time of manufacture.
Long Term Strategies for Gut and Mind Wellness
- Keep your diet clean and colorful
- Manage stress daily
- Stay active and sleep well
- Supplement smartly
- Listen to your body
Signs Your Gut is Healing
- Better digestion
- Improved mood
- More energy
- Clearer skin
- Fewer cravings
When to See a Professional
Recognizing Red Flags
- Persistent bloating or gas
- Unexplained fatigue or mood swings
- Autoimmune symptoms
- Frequent infections
Conclusion
Your gut isn’t just where digestion happens it’s a command center for your entire mental and emotional well-being. By nurturing your gut, you’re not just healing your stomach; you’re creating the foundation for a clearer mind, calmer emotions, and a more joyful life. It’s not a magic pill but with patience, consistency, and the right choices, healing is absolutely possible from the inside out.

 Medically reviewed by
Medically reviewed by